In the heart of Europe, a silent battle is raging, one that threatens to disrupt not just public health but also the agricultural and energy sectors. A recent study published in the journal ‘AIMS Microbiology’ (which translates to “Ambition, Innovation, and Motivation in Microbiology”) has shed light on the alarming rise of antibiotic resistance (AR) in Gram-negative bacteria across the Western Balkans and Hungary. The research, led by Chioma Lilian Ozoaduche from the Agribiotechnology and Precision Breeding for Food Security National Laboratory at the Hungarian University of Agriculture and Life Sciences, offers a stark reminder of the interconnectedness of human, environmental, and animal health—a concept known as the One Health approach.
The study focuses on three notorious bacteria: Pseudomonas aeruginosa, Escherichia coli, and Acinetobacter baumannii. These microbes have been found to harbor a plethora of resistance genes, including those that confer resistance to last-resort antibiotics like carbapenems. “The distribution of these resistance genes is not just a health concern but also an economic one,” Ozoaduche explains. “The energy sector, particularly bioenergy production, relies heavily on microbial processes. Resistant bacteria can disrupt these processes, leading to significant financial losses.”
The research highlights the prevalence of high-risk clones, such as P. aeruginosa ST235 and E. coli ST131, which have been found in both clinical and environmental settings. These clones’ adaptability and widespread dissemination underscore the urgent need for systematic infection control practices. “The adaptability of these bacteria is a testament to their resilience,” Ozoaduche notes. “They can thrive in diverse environments, from hospitals to agricultural fields, making them a formidable foe.”
The commercial implications are profound. In the energy sector, bioenergy production often involves microbial fermentation processes. Resistant bacteria can disrupt these processes, leading to inefficiencies and increased costs. Moreover, the use of antibiotics in agriculture to combat resistant bacteria could have unintended consequences, potentially exacerbating the resistance problem.
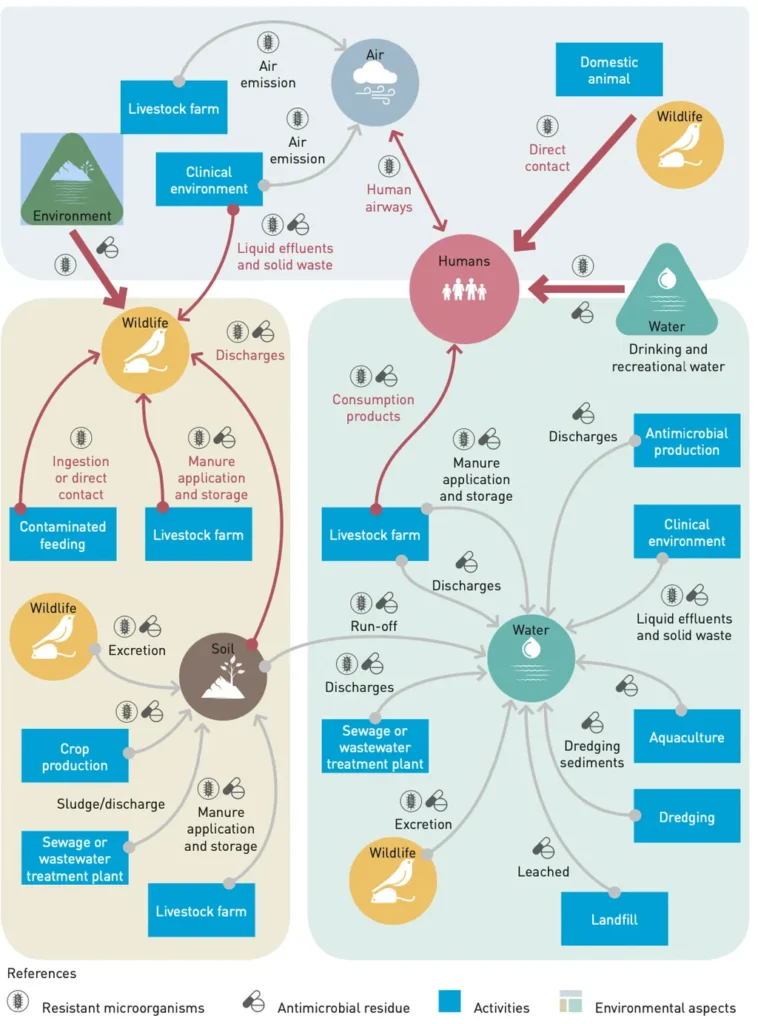
The study also emphasizes the need for further research from a One Health perspective. This holistic approach recognizes the interconnectedness of human, animal, and environmental health, and it’s a perspective that the energy sector would do well to adopt. By understanding the complex interplay between these domains, we can better combat the spread of antibiotic resistance and mitigate its economic impacts.
As Ozoaduche concludes, “This research is a call to action. We need to adopt a One Health approach to combat antibiotic resistance. The stakes are high, not just for public health but for the economy as well. The energy sector, in particular, has a vested interest in this fight. Together, we can turn the tide against this silent but formidable enemy.”